Having your baby admitted to the NICU is never planned. It can be a scary time with a lot of unknown. It is important to remember that your baby is getting the care they need and you can lean on friends and family for support. Hopefully our NICU/Pre-term guide will make this part of your parenting journey a little bit easier.

“These truly amazing people (in the NICU) are attuned to the healthy development of these children and their powerfully peaceful care was life-changing for my baby. In many ways, I feel he is fortunate to have entered life being loved by so many exceptionally compassionate people. The day he graduated and came home with us was just as earth shattering as the day he was born. Know that you have great joy on its way to you!”
-Mom of pre-term baby in the NICU
Neonatal Intensive Care Unit (NICU)
is sometimes also called a specialty care unit, an intensive care nursery, and newborn intensive care. The purpose of the NICU is to care for pre-term or ill newborn babies. Typically the team of experts in the NICU consists of neonatologists, and specially-trained NICU nurses, occupational therapists, physical therapists, speech therapists and respiratory therapists.
Most Common Reasons for Admission to NICU:
Pre-term birth – Baby born before 37 weeks gestation.
Difficulty during delivery
Respiratory Distress Syndrome (RDS) – Baby is having difficulty breathing
Jaundice – High level of bilirubin in the blood indicating increased blood cell breakdown. Babies with jaundice usually need phototherapy.
Sepsis – Infection that spreads throughout blood and body tissue.
Transient Tachypnea of the Newborn (TTN) – Rapid breathing of more than 60 breaths per minute for more than 4 hours after birth.
Apnea – Pause in breathing for more than 20 seconds.
Bradycardia – Abnormal slowing of the heart rate.
Bronchopulmonary Dysplasia (BPD) – chronic lung disease
Other considerations such as Down syndrome, feeding difficulties, anemia, issues with bowels and other conditions.

“I feared because it was too early, I cried because it was too soon. Yet I underestimated the strength in one as small as you.”
-Unknown
Equipment in the NICU
There is a lot of equipment in the NICU but try not to be intimidated by it. It is all there to help your baby grow and get well so they can go home. It is helpful to learn what each piece of equipment is for and how it assists your baby. This guide is helpful, but you can also ask your nurse, therapist or neonatologist in the NICU to explain it all to you.
- Incubators: These are small temperature-controlled beds enclosed by clear, hard plastic to keep your baby warm until they learn to control their own temperature. You can open the tiny windows and talk to your baby and put your hands inside.
- Infant warmers: These are small open beds with heaters over them to help babies stay warm.

- Phototherapy: Phototherapy is a light blanket or a light over the bed to treat jaundice.
- Feeding tubes: Babies born premature are often unable to suck and swallow on their own right away, so they are fed through a feeding tube. Feeding tubes enter through the mouth or nose and go into a baby’s stomach. They are taped in place so the baby does not pull them out. Nurses often change the tubes from one side to the other to prevent soreness.
- Intravenous Catheter (IV): An IV is a very thin, pliable tube that goes into a vein to give medicines and fluids. IVs are usually are in the hands or arms, but some babies have them in other places, like the feet, legs, or scalp.
- Lines. Some babies need to get greater amounts of fluids and medicines than an IV can provide. They get larger tubes called central lines put into a large vein in the chest, neck, or groin. Surgeons put in central lines. Arterial lines are placed in arteries, not veins. They’re used to check blood pressure and oxygen levels in the blood (but some babies may not need a line and they will have a blood pressure cuff instead).
- Umbilical Venous Catheter (UVC): A UVC is a thin, pliable tube that is put into a blood vessel in the baby’s belly button. It can be used to draw blood or to administer fluids and medicine quickly.
- Ventilators: A Ventilator is a machine that helps a baby breath. A baby is connected to the ventilator by an endotracheal tube (a plastic tube placed into the windpipe through the mouth or nose). Sometimes babies who’ve been in the NICU for several months may have a tracheostomy (a plastic tube put into the windpipe) that’s connected to the ventilator on the other end.
- Continuous Positive Airway Pressure (CPAP) or nasal cannula: Some babies need extra oxygen but don’t need
 a ventilator. Babies who can breathe on their own might just need a little extra oxygen support from plastic tubes in the nose (nasal cannula) or from a CPAP machine.
a ventilator. Babies who can breathe on their own might just need a little extra oxygen support from plastic tubes in the nose (nasal cannula) or from a CPAP machine. - Monitors: Monitors let nurses and doctors keep track of your baby’s vital signs (things like temperature, heart rate, and breathing) from any place in the NICU. Monitors include:
- Chest leads: These small, painless stickers on your baby’s chest have wires that connect to monitors. They track heart rate and number of breaths.
- A pulse oximetry (Pulse Ox): This machine measures your baby’s blood oxygen levels. Also painless, the pulse ox is taped to your baby’s fingers or foot like a small bandage and emits a soft red light.
- A temperature probe records your baby’s temperature and shows it on the monitor. This is a coated wire placed on your baby’s skin with a patch.
- Blood pressure is monitored through an arterial line or a blood pressure cuff.

What your NICU baby wants you to know:
Having a baby in the neonatal intensive care unit (NICU) can be a scary, emotional experience! As an occupational therapist in the NICU, I interviewed some babies in the NICU and this is what they would like mommy and daddy to know:
- I feel your energy as soon as you approach me.
As you approach to the incubator, think about the energy that you carry. Babies are very perceptive. Are you stressed, anxious, nervous or hurried? Your baby will sense this. Take a deep breath before you approach your baby so you can be calm and serene as you come into their world. Talk with a loving, low voice, use gentle touch, and reassure your baby that you are calm and ready to care for them.
- I cannot process too much information at once.
Babies are working very hard to take in all the information from their world. They need to process what they see, hear, feel, and taste all at once and it is easy for them to become overstimulated. If your baby is focusing on your face and they are visually stimulated, limit noise and movement and touch. If you are rocking or stroking baby, limit all other stimulation and if you are talking to the baby and they seem to be focusing on your voice, limit touch, movement and visual stimulation.
taste all at once and it is easy for them to become overstimulated. If your baby is focusing on your face and they are visually stimulated, limit noise and movement and touch. If you are rocking or stroking baby, limit all other stimulation and if you are talking to the baby and they seem to be focusing on your voice, limit touch, movement and visual stimulation.
- I can smell you coming.
Babies sense of smell is very well-developed at birth and they are calmed by mommy’s scent. Consider leaving an article of clothing that you just wore with you baby when you leave. You could also put a small burp cloth against your skin, then leave it with your baby when you are not there to keep your baby calm.
- I need skin to skin touch.
Kangaroo care (putting baby down mommy or daddy’s shirt against the skin) is great for baby’s development and for bonding with the baby. This helps to regulate baby’s temperature, heart rate, respirations, and brain development. You can also do baby massage for skin on skin contact. The developmental benefits of skin on skin contact are immeasurable!
- I feel calm when I hear familiar sounds.
Babies are able to hear in utero and by recreating the sounds of utero, babies can be soothed. Mom’s voice is usually very calming for baby. Sing to your baby, read a book, and just talk to your baby. Studies show that babies demonstrate familiarity to mom’s voice just one day after birth. Babies are also calmed by white noise or ocean sounds, recreating the swishing sound of the amniotic fluid. Babies also like the sound of the heartbeat and many baby sound machines play a heartbeat sound.
It can be very difficult to have a baby in the NICU, but remember, they are getting the care they need and you can take advantage of the knowledge of the nurses, therapists and neonatologists to give you support and information before you bring your precious baby home.

Prematurity Corrected Age Calculation:
If your baby was born premature, there are two important dates in your life. Your baby’s actual birthdate and your baby’s due date. When considering developmental milestones, you will subtract the amount of weeks that your baby was preterm to determine her actual developmental level. For example, if a four-month old, was born two months early, we would expect him to be at the developmental level of a two-month-old, not a four-month-old. We would expect him to be hitting the milestones of a two-month-old, not a four-month-old.
 The Neonatal Research Institute has an actual calculator on their site you can use to determine your baby’s corrected age. You don’t really need a calculator, though. It is simple math.
The Neonatal Research Institute has an actual calculator on their site you can use to determine your baby’s corrected age. You don’t really need a calculator, though. It is simple math.
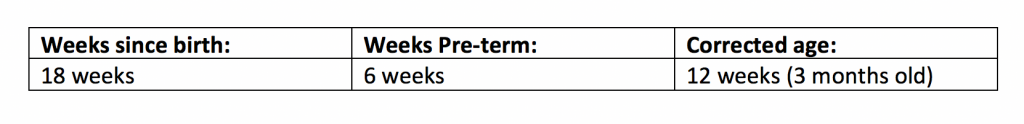
Simply take your baby’s actual age in weeks or months (how long since birth) and subtract the number of weeks your baby was pre-term. To determine how many weeks pre-term your baby was, subtract their gestational age from 40 because 40 weeks is full term. So, if your baby was born at 36 weeks, 40-36=4. Your baby was born 4 weeks early. So if your baby is 12 weeks old, you would subtract 4 from 12 and your baby’s corrected age is 8 weeks. Even though her chronological age is 12 weeks, you can expect her to be at the developmental level of an 8 week old baby.
Here is another example:
Weeks since birth-weeks pre-term=Corrected age
When you look at your baby’s reflexes and developmental milestones remember to keep the corrected age in mind, not the chronological age.
From Then to Now: Stories from the NICU
Parents of NICU babies share their stories of fear and hope from their days in the NICU along with advice for new parents.






Printable Milestone Cards: